+90-548-875-8000
+90-548-876-8000
Elite Hospital
North Cyprus
Follow Us on
Social Media
Premature ovarian insufficiency (POI) / Failure is when ovaries lose their function before the age of 401. Premature ovarian insufficiency and premature ovarian failure are used synonymously. In fact, the condition used to be referred to as premature ovarian failure previously and more recently this has largely been replaced by the term premature ovarian insufficiency. Perhaps this is because the literal meanings of these terms correspond to two different points along the infertility spectrum.
Insufficiency is when the ovarian activity is much lower than expected for a certain age bracket. In cases of insufficiency, it may still be possible for a woman to get pregnant either naturally or via IVF treatments. Failure, on the other hand, refers to a final state where the ovaries are no longer active and pregnancy is no longer possible. In a way, we can think of insufficiency as a fertility status that leads to ovarian failure, possibly in a short period of time.
Ovarian insufficiency means the typical hypothalamus-pituitary-ovary axis does not work as well as it should and expected follicular development doesn’t take place. As a result, when follicles don’t grow, they don’t release estrogen. A low level of estrogen compromises both the ovarian cycle as well as endometrial growth. Premature ovarian insufficiency, therefore, is a major issue in terms of infertility.
POI is most likely to occur spontaneously without any specific cause and it can affect up to 4% of women2. Even though it doesn’t have a specific cause that can be easily identified in most of the cases, there are some known causes which are associated with the condition. These include3:
Women who are experiencing premature ovarian insufficiency are likely to experience symptoms that are secondary to amenorrhea and estrogen deficiency. In most women who present with spontaneous POI, there might be no or very little symptoms, the most common being irregular cycles. In iatrogenic cases, the symptoms may be more severe. This is possibly due to the sudden onset as well as combination of psychosocial aspects as well.
Premature ovarian insufficiency is often considered to be the final step before ovarian failure and premature menopause. Even though there are studies reporting pregnancies in women who experienced premature ovarian insufficiency for years, such incidences are quite low and pregnancy in premature ovarian failure is something that doesn’t happen easily.
One treatment which holds considerable promise for patients experiencing POI is ovarian PRP treatment. Ovarian PRP treatment refers to injection of platelet rich plasma into the ovarian cortices with the expectation of temporary resumption of oogenesis.
Premature Ovarian Failure and Ovarian PRP Treatment
While it was once believed that dormant stem cells in the ovaries could be stimulated into oogenesis and therefore contribute to ovulation and therefore pregnancy, practice has shown that this is more difficult than it is made to be. While technically possible and clinical research is promising, practice with ovarian PRP treatments has shown that primordial follicles are more likely to respond to stimulation with ovarian PRP treatment, compared to stem cells.
Primordial follicles are types of cells that are at earlier stages of oogenesis (development and maturation of the female oocyte (egg)) but for some reason, a great majority of these follicles are destined to waste away. This is the case in women with normal menstrual cycles and ovarian activity. Even though 100s of primordial follicles are prepared for oogenesis, only 1 follicle reaches ovulation in a normal menstrual cycle. The rest of the primordial follicles are simply wasted away. In the early stages of oogenesis, primordial follicles respond to intra-ovarian conditions rather than the gonadotropins. In other words, the role of FSH, LH and the hormonal feedback mechanism is very limited in early stages of primordial follicle development. Rather, growth factors and cytokines present in the ovarian tissue act as signaling mechanisms for differentiation of primordial follicles into pre-antral follicles. Once the primordial follicles reach the pre-antral follicle stage, then they start responding to gonadotropins.
The cytokines that are present in the platelets—TGF superfamily, IGF-1, BMP-4, and BMP-7 can promote folliculogenesis, just like the ones that exist in a healthy ovarian tissue. Similarly, platelets can help establish new blood vessels and promote a healthier environment for oogenesis in general.
Women with POI as well as women in their 40s with declined ovarian function are still likely to have a sufficient population of primordial follicles. This is the principle on which ovarian PRP treatment is built. By injecting the ovaries with the necessary growth factors found in PRP, the primordial follicles are motivated to continue with their differentiation into pre-antral follicles and then viable oocytes. Once this cohort of primordial follicles reach the stage of ovulation approximately 3 months after ovarian PRP treatment, pregnancy becomes possible.
Patients are often recommended to try naturally for three months post-PRP treatment. If pregnancy doesn’t occur within this time frame, then an IVF cycle may be planned, depending on the level of improvement observed in the patient’s ovarian activity.
A number of considerations are worth mentioning with regard to ovarian PRP application:
1- Method
Isolation of the platelets in an optimal concentration is one of the main determinants of success. Apart from obtaining an optimal count of platelets, avoiding spontaneous activation of the platelets is another important step in ovarian PRP application. Platelets should be activated at a precisely calculated time for maximum benefit.
2- Location
Given that ovarian PRP application’s main aim is to stimulate primordial follicles into oogenesis, platelet rich plasma injection should be aimed at the ovarian cortex which is populated by these germline cells. A catheter is loaded with PRP and inserted through the cervix into the ovarian cortex. Once the tip of the cortex is reached, Prof. Savas Ozyigit works backwards to ensure full cortical coverage.
3- Oogenesis
Ovarian PRP treatment aims to stimulate the physiological processes which would naturally take place in the ovaries. In normal female reproductive function, we see primordial follicles differentiating into pre-antral follicles with the help of growth factors and then these pre-antral follicles are stimulated through pituitary hormones into ovulation. In a normal cycle, 100s of primordial follicles are stimulated and only one of them reaches ovulation. The primary aim of ovarian PRP treatment is to commit non-committed primordial follicles into oogenesis.
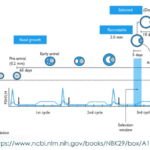
The timeline of female reproduction should be taken into consideration when planning pregnancy after ovarian PRP application. For instance, a primordial follicle will normally take somewhere between 70 to 120 days to reach ovulation. When planning an IVF cycle after an IVF treatment, this should be taken into consideration.
Below is a diagram showing different stages of oogenesis in a timeline:
References:
1. Webber L, Davies M, Anderson R, et al. ESHRE Guideline: management of women with premature ovarian insufficiency. Hum Reprod 2016; 31(5): 926-37.
2. Golezar S, Ramezani Tehrani F, Khazaei S, Ebadi A, Keshavarz Z. The global prevalence of primary ovarian insufficiency and early menopause: a meta-analysis. Climacteric 2019; 22(4): 403-11.
3. Panay N, Anderson R, Nappi R, Vincent A, Vujovic S, Webber L,
Wolfman W. Premature ovarian insufficiency: an International Menopause Society White
Paper. Climacteric 2020; 23(5): 426-4
Please contact us for more detail on Ovarian PRP Treatment.